Health Sciences & Wellness COVID-19 Information and Guidelines
These guidelines are being issued as a supplement to the School of Health Sciences and Wellness’ Policies Handbook (12/10/19 version) to be used for all students and clinical education settings associated with Laramie County Community College’s health programs. Additional guidelines and updates will be provided as needed as the COVID-19 situation evolves and changes.
General Information
Coronavirus Disease 2019 (COVID-19) is a respiratory disease caused by the SARS-CoV-2
virus. This zoonotic virus spread from China to many other countries around the world,
including the United States. This has resulted in COVID-19 being deemed a pandemic.
(CDC, 2020)
The virus is thought to spread mainly from person-to-person, including:
- Between people who are in close contact with one another (within about 6 feet).
- Through respiratory droplets produced when an infected person speaks, coughs, or sneezes. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs.
It may be possible that a person can get COVID-19 by touching a surface or object
that has SARS-CoV-2 on it and then touching their own mouth, nose, or possibly their
eyes. People are thought to be most contagious when they are most symptomatic. However,
there is evidence to show that spread is possible before people show symptoms (pre-symptomatic
transmission). In addition, there have been reports where asymptomatic COVID-19 carriers
have transmitted the disease.
The primary symptoms of COVID-19, which can occur between 2 and 14 days after exposure,
include:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- New loss of taste and smell
- Sore throat
- Fatigue
- Muscle or body aches
- Headache
- Congestion or runny nose
- Some digestive symptoms such as nausea, vomiting, or diarrhea have also been reported.
Individuals diagnosed with COVID-19 can exhibit mild to moderate symptoms, but up to 20% of those infected exhibit severe symptoms and complications, including pneumonia, persistent chest pain or pressure, difficulty breathing, cyanosis, and death. According to the Center for Disease Control and Prevention (CDC) (2020), all individuals are at risk for becoming infected, but current epidemiology studies indicate that older adults (those over age 65) and people of any age who have underlying medical conditions might be at higher risk for severe illness from COVID-19. (www.cdc.gov/coronavirus/2019-ncov)
Currently, there are no vaccines for COVID-19 or drugs to treat the condition once an individual has been diagnosed with the disease; only supportive care can be provided. Therefore, the best methods to fight the spread of this communicable disease are through prevention and strict infection control procedures. For the general population and LCCC students, these prevention procedures include:
- Frequent and thorough hand washing. If soap and running water are not immediately available, provide alcohol-based hand rubs containing at least 60% alcohol
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Staying home if ill
- Completing all required health screening protocols* prior to coming to campus or attending clinical education facilities;
- Respiratory etiquette, including covering coughs and sneezes
- Practice social distancing, remaining at least 6 feet away from another person and avoiding gathering of groups of 25 or more people;
- Wearing face masks or face coverings on campus when social distancing is not possible; and
- Following stay-at-home or other public health orders.
(R2B Plan Phases I and II. www.lccc.wy.edu, 6/2020) *See Appendix A for example health screening questions
Healthcare Workers and Student Clinical Guidance
According to the CDC, healthcare personnel (HCP) refers to, “…all paid and unpaid persons serving in healthcare settings who have the potential for direct or indirect exposure to patients or infectious materials, including body substances; contaminated medical supplies, devices, and equipment; contaminated environmental surfaces; or contaminated air. For this document, HCP does not include clinical laboratory personnel.” (https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html#table1) Based on this definition, students enrolled in one of the Health Sciences and Wellness programs at Laramie County Community College (LCCC) with clinical assignments in healthcare facilities are subject to the same procedures and guidance followed for the employees of their clinical sites.
For healthcare workers, spread of the SARS-CoV-2 virus is thought to occur mostly from person-to-person via respiratory droplets among close contacts. Close contact for healthcare exposures is defined as follows: NEW as of 10/21/2020: Any individual within 6 feet of a laboratory-confirmed or probable COVID-19 patient for a cumulative total of 15 minutes or more over a 24- hour period. This could occur in various settings such as caring for or visiting the patient; or sitting within 6 feet of the patient in a healthcare waiting area or room); or b) having unprotected direct contact with infectious secretions or excretions of the patient, including sputum, serum, respiratory droplets, and blood (i.e., being coughed on, touching used tissues with a bare hand). (www.cdc.gov, 2020) (CRMC COVID-19 Guidance 5/2020) Laramie County Health, Casey Mullins, RN, email, 9/14/2020; www.cdc.gov; https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/appendix.html#contact10/21/2020
Infection Control in Healthcare
In addition to the infection control procedures for the general public discussed earlier, healthcare facilities are actively taking additional steps based on CDC recommendations to prevent the transmission of COVID-19 using three primary approaches:
- Limiting how pathogens enter the facilities: These include measures such as limiting entrances, screening patients for respiratory symptoms, encouraging respiratory hygiene in the facility, the increased use of telemedicine, and the cancellation of elective or non-critical procedures.
- Isolating symptomatic patients as soon as possible: Many facilities have reconfigured their entrances, waiting rooms, and treatment areas to place patients with COVID-19 or suspected COVID-19 in separate areas or different buildings altogether. COVID-19 patients must be provided with a mask upon entering the facility, and if admitted, must be placed in private rooms--and a private bathroom, whenever possible.
- Protecting healthcare personnel: These measures include an emphasis on hand hygiene, creating barriers to the triaged entrance area, placing COVID-19 patients in separate areas of the facility, limiting the number of staff providing care for COVID-19 patients, prioritizing and limiting aerosol-generating procedures, and implementing Personal Protective Equipment (PPE) procedures and strategies, adhering to standard and transmission-based precautions. https://www.cdc.gov/coronavirus/2019-ncov/infection-control
It is for the reasons above that several clinical education centers made the decision
in March 2020 to not host LCCC students for an indefinite period. With more testing
and monitoring now available, many clinical facilities are now allowing students to
resume their clinical experiences. However, student assignments may still be subject
to change if COVID-19 cases begin to increase, if public health orders change, and/or
based on individual facility circumstances and resources. Each HSW health program
will continue to monitor their accrediting bodies’ policies and their clinical sites’
policies and availability so that students are able to complete their programs as
expediently as possible.
When students re-enter their clinical rotation assignments, the following principles
should be considered:
- Because the physical layout and workflow of the clinical site and specific clinical assignment area may have changed due to the facility’s revised infection control procedures, clinical sites are expected to provide an orientation to all students regarding their COVID-19 containment measures, their expectations of student participation in potential COVID-19 patient interactions, and the expected PPE and infection control protocols.
- To maintain social distancing, students are expected to maintain a distance of at least 6 feet from others whenever possible. In addition, congregating in groups is discouraged (i.e., cafeteria, lobbies, and waiting rooms.)
- Generally, students have not been routinely assigned to patients kept in Isolation, and with the recent rapid spread of COVID-19 and the limited supply of personal protective equipment (PPE), it is likely that students will also not be routinely assigned to directly care for patients diagnosed with COVID-19. However, this will vary with each facility’s protocols and each program’s clinical assignments, and this can still place a student in the medium-risk of exposure, based on OSHA guidelines (OSHA, 2020). Workers with a medium exposure risk may still need to wear some combination of gloves, a gown, a face mask, and/or a face shield or goggles. CDC instructions for donning and doffing PPE may be found at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/using-ppe.html. A video tutorial for putting on PPE is available from the CDC at: https://youtu.be/of73FN086E8.
- Recognizing that a student’s exposure risk could be medium to high, depending upon their clinical assignment, students are required to strictly follow their facility’s COVID-19 infection control and PPE guidelines.
- Because COVID-19 is a respiratory illness, face coverings serve as the most commonly
worn type of PPE in health care facilities. Face masks will be worn each clinical
day and students are expected to follow these general guidelines:
a. Students will be required to wear a surgical mask and eye protection (either face shields or safety glasses with side shields) during clinical hours and in all patient care and public areas as specified by the clinical site;
b. Ideally, disposable masks will be disposed of after each day of clinical, or anytime the mask becomes wet or soiled. However, due to PPE shortages, a surgical mask that remains dry and unsoiled may be worn for a period of up to one week (three to five clinical or lab days.) Students may also wear a cloth mask over the surgical mask for additional protection and/or to extend life of mask if clinical policies allow. Cheyenne Regional Medical Group and Cheyenne Regional Physicians Group: email correspondence; 9/10/2020
c. Cloth masks must be laundered daily using detergent, hot water, and dried using the highest heat setting. CDC guidelines for appropriate laundering are available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-to-wash-cloth-face-coverings.html;
d. Safety glasses and face shields issued to students that remain in working order or are not visibly damaged or difficult to see through may be worn throughout the student’s clinical experience. CDC guidelines for appropriate cleaning of eye protection can be found at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/eye-protection.html.
e. If a student has been issued an N-95 mask, the clinical site may require proof of proper fit-testing;
f. Clinical policies may be more stringent than outlined here; in these cases, clinical policy will prevail. Students are advised to check with their clinical instructors on the required face coverings at their respective clinical sites.
g. If a student fails to arrive with or follow the clinical site’s face mask or PPE protocols, the student may be sent home and an absence or tardy may be documented using each program’s clinical attendance policies.
- Due to the limited availability of PPE, a clinical site may ask individual programs to supply the necessary PPE for the students assigned to their site. LCCC will make every effort to comply with these requests. In the event that the request cannot be met, a student may need to be re-assigned to another alternative site.
COVID-19 Exposure Documentation and Clinical Attendance Guidelines
Because of their potential frequent and close contact with vulnerable individuals in healthcare settings, CDC guidelines recommend that healthcare workers and students are also responsible for monitoring themselves to quickly identify early COVID-19 symptoms and prevent transmission to patients, other healthcare workers, and visitors. If a student develops signs of a respiratory condition (fever, sore throat, cough, or shortness of breath), they should not attend clinical while they exhibit any of these symptoms, following the normal clinical absence notification procedures of the applicable program. Individual programs are encouraged to develop or revise their clinical attendance policies to prevent the spread of COVID-19.
Health Monitoring
As part of Laramie County Community College’s Phase II Return to Business Plan, all students and faculty are required to complete the Eagle Health Screening questionnaire for any LCCC-related activity, including clinical. This screening is to be completed prior to coming on campus for any in-person classes, labs, or other LCCC business, or before arriving at an off-campus clinical site. The Eagle Health Screening questionnaire may be accessed in myLCCC using the Eagle Health Screening app or by scanning the QR Code shown in Appendix B. Once all of the answers to the questionnaire are submitted indicating that no COVID-19 symptoms or conditions are present, the student or faculty member will receive a confirmation email stating they are cleared to come to campus (or the clinical site, as applicable.)
If a confirmation email is not received or an email is received stating that the student or faculty member is not cleared to come to campus (or clinical), students and faculty should NOT attend their on-campus or off-campus clinical sites and are advised to contact the appropriate instructor for absence notification and further instructions. The Dean of Students will also receive notification through this electronic system. LCCC faculty will need to notify their immediate supervisor and LCCC’s Human Resources Office will be contacted.
In addition to LCCC’s Eagle Health Screening, each HSW health program will determine the clinical clearance requirements and screening frequency that meet their needs and their clinical facilities’ needs. In general, most clinical facilities require that all health screening criteria are met (i.e., that no symptoms of COVID-19 are present) each day the student attends clinical. Clinical sites may also require the completion of their health screening protocols in addition to those required by LCCC; some facilities may also require the documentation of normal temperature readings prior to a clinical assignment.
To document that students are meeting the COVID-19 health monitoring requirements of clinical facilities, the LCCC Health Sciences and Wellness (HSW) School has contracted with CastleBranch* to electronically record this information in addition to the student’s immunization, drug screening, and background check account. This new module includes questionnaires regarding exposure to COVID-19, symptoms, educational training on infection control and proper handwashing techniques, and a daily temperature log.
* Individual programs may have health monitoring requirements with other vendors as a requirement of their program in addition to, or in lieu of CastleBranch. Check with your program for their requirements.
Temperature Monitoring:
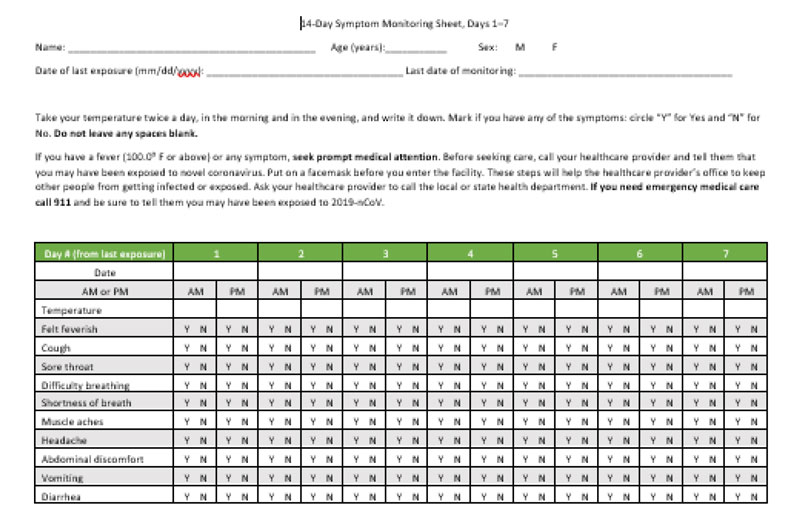
To comply with CDC and clinical policies, daily temperature monitoring is required under the following circumstances:
- The student or faculty member is assigned to a clinical site that mandates this as a condition for student assignment at its clinical facilities;
- The student’s educational program is requiring this health monitoring component; and/or
-
The student has been exposed to COVID-19, either in the clinical setting or through a personal contact (a family member or friend), and is completing the required 14-day quarantine period. (See pages 6-7 regarding COVID-19 Exposure.)
Temperature Monitoring Instructions: Students are expected to take their temperature with an electronic thermometer two times a day, once in the morning, and again in the evening. If you do not have an electronic thermometer, please let your Clinical Coordinator and/or Program Director know as soon as possible. It is recommended that the temperature be taken at the same times each day, and that they are not taken immediately after any meals or beverages. Record each reading in the CastleBranch website form (and/or the applicable clinical facility’s form) as soon as possible.
Please also note the following policies and procedures regarding this health requirement. Any temperature reading 100 degrees F or higher:
-
- Will light up in red on the CastleBranch record;
- Prevents you from attending clinical or an on-campus class or lab;
- Must be reported to the appropriate program representatives and/or your clinical instructors/preceptors;
- Must also be documented on that day’s health screening questionnaire as appropriate; and
- Will require further medical intervention. Students will need to call their primary care provider for further guidance, testing, and treatment.
Students are advised that the failure to complete any of their program’s required health screenings in an honest and timely manner may prevent or delay their clinical placement and students may also be subject to disciplinary action, up to, and including, program dismissal. The inability to obtain the necessary clinical hours and/or competencies may also prevent or delay the student’s completion of the applicable clinical course and/or the program.
Exposure Reporting
If Exposure Occurs At the Clinical Setting: In support of the Standard Health and Safety Practices and Exposure Guidelines outlined in the Health Sciences and Wellness Policy Handbook on pages 9-11, student exposure to COVID-19 should be handled as follows: In the event that a student is exposed to the COVID-19 virus as a result of their clinical assignment, this should be reported immediately to their on-site clinical instructor/preceptor, the program’s Clinical Coordinator (if applicable), and the Program Director. An Incident Report or other documentation will be completed; a meeting with the facility’s Infection Control and/or Occupational Health staff may also be required. At a minimum, the following information should be included in the exposure report as recommended by the recent Infection Control for Healthcare Personnel document published by the CDC in October 2019, “…Include(ing) where, when, and how the exposure occurred, the duration and extent of the exposure, and whether appropriate PPE was used and functioned correctly.” (https://www.cdc.gov/infectioncontrol/pdf/guidelines/infection-control-HCP-H.pdf, p.40) This information can then be used to determine the need for further follow-up and testing for the virus.
Testing for the virus will follow the clinical site’s protocol for documented COVID-19 exposures. As outlined in Current guidance from the CDC have established the following testing guidelines based on the type of exposure and the symptoms presented:
- Critical infrastructure workers, healthcare workers, or first responders may need to get tested according to your employer’s or clinical site’s guidelines for the purposes of surveillance testing or if displaying symptoms of COVID-19;
- Health Sciences and Wellness students with COVID-19 symptoms are required to complete the Eagle Health Screening and notify the Dean of Students and program faculty. Students will be advised to see their healthcare provider for testing;
- Any individual who has been in close contact, such as within 6 feet of a person with a confirmed or probable SARS-CoV-2 infection for at least 15 minutes over a 24-hour period even if they do not have symptoms.
https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html (9/21/2020, 10/23/2020)
The risk of the exposure is based on the type and extent of contact and the presence of PPE as outlined in the following link: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-risk-assesment-hcp.html#table1.
The presence and type of PPE and the location of the exposure are used by Public Health Officials to determine whether a quarantine period is necessary as outlined by the two scenarios provided below:
- “When a student is in a classroom or lab setting, the student needs to try to maintain 6 feet of social distancing. If unable to maintain the 6 feet they must wear a mask. It does not matter the type of mask in this setting as they will be quarantined if they meet the definition of close contact (6 feet x 15 cumulative minutes). While in the role of the “Student” they are not exempt from quarantine.”
- “When a student is in a clinical setting/ healthcare agency (i.e VA, CRMC, or CRG) the student needs to wear a surgical mask not a cloth mask. If they are in an aerosolized procedure, they must wear a N95 and Eye protection. If they are exposed and the positive is also wearing a surgical mask, the student will not be quarantined as they fall into the Healthcare Provider role. If the positive is not wearing a mask, the student would need to have on a mask and eye protection. If not wearing both, the student will be quarantined.” (Laramie County Health, Casey Mullins, RN, 9/9/2020 email correspondence)
Due to these guidelines, all students in clinical experiences will wear surgical masks and eye protection during their clinical rotations as outlined on page 4 of this policy.
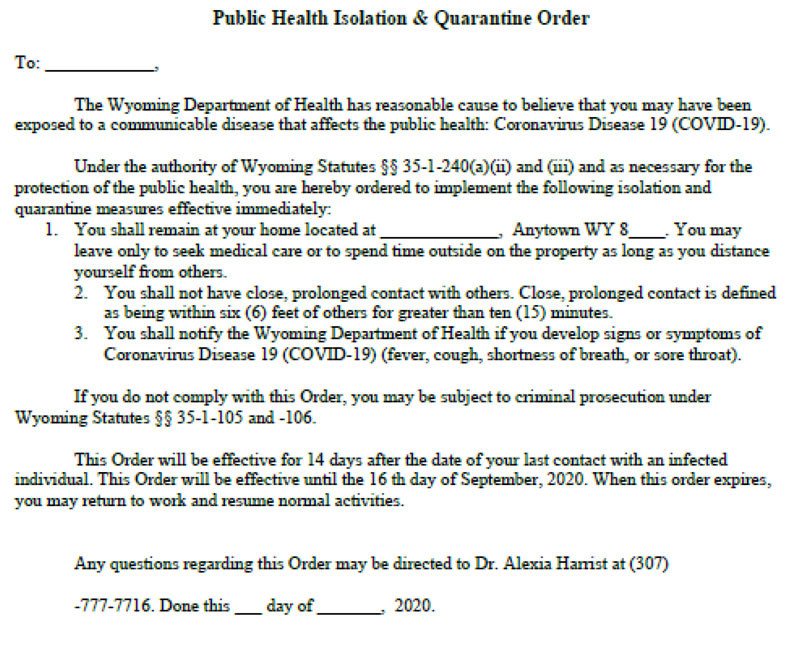
Quarantine/Isolation Orders
Once an individual has tested positive for the COVID-19 virus, public health officials begin a process called contact tracing. Laramie County Health is responsible for conducting contact tracing for Laramie County Community College. Once they receive the positive test result from their lab or from the State of Wyoming Health Department, they will call the individual to ask about all close contacts the individual has had in the 48 hours prior to the positive test or the onset of symptoms, if symptoms were present prior to the test. The positive individual will also be sent Health Orders from the State of Wyoming (or the respective state) to remain home, isolating themselves from others for the duration of the order, which can be a period of 10 to 14 days.
Based on the information provided by the COVID-positive individual, the public health official will make the determination of the individuals who meet the definition of close contacts, and who will need to therefore be issued quarantine orders. They will call each individual to notify them of their exposure to COVID-19 due to the close contact which occurred, and they will advise the affected contacts to remain home, avoiding close contact with others for a period of up to 14 days. They are also issued a stay-at-home quarantine order by the State of Wyoming (or respective state.) An example of a quarantine order is available in the Appendix. Quarantined individuals will also be advised to monitor themselves for COVID symptoms, including recording a temperature reading twice a day. (An example of a symptom monitoring chart is provided in the Appendix.) If they develop symptoms, they are advised to contact the public health office and seek medical care if symptoms become severe. Close contacts who become symptomatic are then considered probable cases, and are logged as such, even if no test is conducted. It is important to note that only a Public Health Officer can issue quarantine orders.
The preferred method for student screening if an exposure has occurred is testing for the virus. If testing is available, a period of 7-10 days with temperature and symptom monitoring may still be necessary due to the incubation period of the virus, and this guidance will be provided by the Public Health Officer. If the test is positive, or the student has been issued a quarantine stay-at-home order, the student is not to attend any in-person classes or clinical and the Clinical Coordinator and/or Program Director and the Dean of Students must be notified. Notification to the Dean of Students may be completed by filing a CARE Team Report with the required documentation or calling 307.778.1223.
After the Dean of Students verifies the COVID-related illness and/or quarantine order, an Excused Absence email will be sent to all of the faculty of the courses that the student is enrolled in and the associated Academic Dean(s). It is important to note that an Excused Absence issued in this case:
- Applies only to COVID-19. Other illnesses and students waiting for COVID test results will be handled following each program’s existing illness and absence policies.
- Starts from the date and time that the Dean of Student’s email is sent/received
- Extends for as long as fourteen days (or as long as the isolation or quarantine order is in effect.)
- Does not pre-empt program policies for competency completions and other professional expectations.
If a student has a positive test or has been issued a quarantine order, the student will be excused from all face-to-face clinical and on-campus activities for the duration of the illness/quarantine. If it has been determined that students or faculty members may have been exposed to a positive COVID individual due to positive COVID-19 test results received by the Dean of Students’ Office, the Dean of Students’ Office and/or HR will contact the affected faculty and students and recommend COVID-19 testing. They will also provide information about obtaining and completing a test. (LCCC Dean of Students, 10/21/2020.)
Students and faculty may return to clinical once the quarantine order expires or when they are symptom-free as follows using CDC guidelines: At least 24 hours have passed since the last fever without the use of fever-reducing medications and improvement in respiratory symptoms (e.g., cough, shortness of breath) AND at least 10 days have passed since symptoms first appeared. Please be advised that at this time, LCCC is requiring a physician’s note be provided to Human Resources (for LCCC employees) or the Dean of Students (for students) to return to campus.
Clinical sites may also require this type of documentation in order to resume clinical experiences and/or may require wearing a medical face mask at the site until all respiratory symptoms, if present, have dissipated. In addition, clinical sites may require a letter from the program verifying the student is cleared to return to the clinical setting. In this case, a letter from the Program Director to the clinical site listing the day after the quarantine period has expired will suffice. R2B Plan Phase 1 and 2. www.lccc.wy.edu; https://www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/hcp-return-work.html; Dean of Students and Clinical Correspondence, September 2020.
As outlined in the Health Sciences and Wellness Policy Handbook on page 9, it is highly recommended that students carry their own health insurance. If a student requires treatment, clinical site policy will prevail, and all costs are the responsibility of the student.
If Exposure Occurs Outside the Clinical Setting: If a student has been in close contact with an individual outside of clinical (i.e., a friend or family member) who tests positive for COVID-19, they must answer “yes” to the close contact question on the daily Eagle Health Screening, and report this to the program’s Clinical Coordinator (if applicable), and the Program Director as soon as possible. The Dean of Students must be notified, and the student will not be allowed to participate in in-person activities, clinical, or labs, but synchronous online participation or virtual learning activities should be used as much as possible. In this case, the exposed individual should be contacted by Public Health within 48 hours. If, at the end of 48 hours, no contact has come from the Public Health Office, the student may call the county or State Health Office to determine if the individual they believe they were exposed to is on the list of positive cases. If the answer is “yes,” the Public Health Office will provide the quarantine orders and other instructions at that time. If the answer is “no,” the individual should follow the instructions provided by the public health officer, which may include a full return to in-person activities.
To illustrate the use of quarantine and testing in the event of an exposure occurring due to close contact with a COVID-positive individual, testing for the virus can still be used to clear the student for clinical or class participation. However, the source of the exposure can affect the quarantine period as outlined below:
Exposure occurs and is NOT considered a healthcare worker exposure and is NOT due to a household member
If testing is available, a self-quarantine period of 7-10 days with temperature and symptom monitoring is recommended due to the incubation period of the virus. If the test is positive, the Public Health orders for a positive test will be followed. If the test is negative, the student may return to clinical and/or campus for in-person activities, providing this documentation to the program’s Clinical Coordinator and/or Program Director (and the Dean of Students.)
Exposure occurs due to a household member
- If testing is available and the household member is being tested, the student will follow Public Health orders which will typically include quarantine and self-monitor for symptoms until the family member’s test results are available. If the family member’s test results are negative, the student may return to clinical and other in-person activities, providing the necessary documentation to both the Dean of Students and the Program Coordinator/Director for appropriate clearance.
- If the family member’s test is positive, the student will be required to quarantine for the period of time required by public health officials (which may be as long as 14-days) and self-monitor for symptoms.
Programs are advised to also document student self-reported exposures and their results or resolution that may have occurred when LCCC classes were/are not in session.
Thank you for your assistance in assuring the health and safety of the LCCC Health Sciences and Wellness community and the patients and stakeholders we serve. Everyone is responsible for containing the spread of the coronavirus by complying and cooperating with all public health orders, public health officer and healthcare provider recommendations regarding their exposure and/or potential exposure, and any contact tracing efforts regarding potential exposure.
Resources
The U.S. Department of Health and Human Services’ Centers for Disease Control and Prevention (CDC) provides the latest information about COVID-19 and the global outbreak at: www.cdc.gov/coronavirus/2019-ncov.
The OSHA COVID-19 webpage offers information specifically for workers and employers at: www.osha.gov/covid-19.
The State of Wyoming’s Public Health Office and Updated Orders for COVID-19 are available at: https://health.wyo.gov/publichealth/infectious-disease-epidemiology-unit/disease/novel-coronavirus/
University of Colorado-Health Coordinator of Education Programs (Anetria Cain): studentsuchealthnorth@uchealth.org; June 2020
Banner Health Western Division Hospitals – Education Systems Notification (myClinical Exchange) June 2020
Ivinson Memorial Hospital – Student Pandemic Safety Precautions (Ivan Olson) June 2020
Cheyenne Regional Medical Center, Occupational Health (Darrallynn Patterson) June 2020
Return2Business Phases I and II; Laramie County Community College; June/July 2020.
Laramie County Health, Casey Mullins, RN, email, 9/14/2020
Dean of Students and Clinical Correspondence, September 2020, October 21, 2020
https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html (9/21/2020)
https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/eye-protection.html.
Cheyenne Regional Medical Group and Cheyenne Regional Physicians Group: email correspondence; 9/10/2020
Appendix A
Appendix B